Search
- Page Path
- HOME > Search
- Thyroid
- It Is Time to Understand the Additional Benefits of Active Surveillance for Low-Risk Papillary Thyroid Carcinoma
- Kyeong Jin Kim
- Endocrinol Metab. 2024;39(1):95-97. Published online February 22, 2024
- DOI: https://doi.org/10.3803/EnM.2024.104
- 779 View
- 37 Download

- Diabetes, Obesity and Metabolism
- Sleep Duration and the Risk of Type 2 Diabetes: A Community-Based Cohort Study with a 16-Year Follow-up
- Da Young Lee, Inha Jung, So Young Park, Ji Hee Yu, Ji A Seo, Kyeong Jin Kim, Nam Hoon Kim, Hye Jin Yoo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Seung Ku Lee, Chol Shin, Nan Hee Kim
- Endocrinol Metab. 2023;38(1):146-155. Published online February 6, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1582
- 2,617 View
- 165 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
We aimed to investigate the moderating effects of obesity, age, and sex on the association between sleep duration and the development of diabetes in Asians.
Methods
We analyzed data from a cohort of the Korean Genome and Epidemiology Study conducted from 2001 to 2020. After excluding shift workers and those with diabetes at baseline, 7,407 participants were stratified into three groups according to sleep duration: ≤5 hours/night, >5 to 7 hours/night (reference), and >7 hours/night. The Cox proportional hazards analyses were used to calculate the hazard ratios (HRs) and 95% confidence intervals (CIs) for incident type 2 diabetes mellitus (T2DM). Subgroup analyses were performed according to obesity, age, and sex.
Results
During 16 years of follow-up, 2,024 cases of T2DM were identified. Individuals who slept ≤5 h/night had a higher risk of incident diabetes than the reference group (HR, 1.17; 95% CI, 1.02 to 1.33). The subgroup analysis observed a valid interaction with sleep duration only for obesity. A higher risk of T2DM was observed in the ≤5 hours/night group in non-obese individuals, men, and those aged <60 years, and in the >7 hours/night group in obese individuals (HRs were 1.34 [95% CI, 1.11 to 1.61], 1.22 [95% CI, 1 to 1.49], and 1.18 [95% CI, 1.01 to 1.39], respectively).
Conclusion
This study confirmed the effect of sleep deprivation on the risk of T2DM throughout the 16-year follow-up period. This impact was confined to non-obese or young individuals and men. We observed a significant interaction between sleep duration and obesity. -
Citations
Citations to this article as recorded by- Attention to Innate Circadian Rhythm and the Impact of Its Disruption on Diabetes
Da Young Lee, Inha Jung, So Young Park, Ji Hee Yu, Ji A Seo, Kyeong Jin Kim, Nam Hoon Kim, Hye Jin Yoo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Nan Hee Kim
Diabetes & Metabolism Journal.2024; 48(1): 37. CrossRef - Role of Sleep and Sleep Disorders in Cardiometabolic Risk: a Review and Update
Shaden O. Qasrawi, Ahmed S. BaHammam
Current Sleep Medicine Reports.2024; 10(1): 34. CrossRef - Evaluating reliability in wearable devices for sleep staging
Vera Birrer, Mohamed Elgendi, Olivier Lambercy, Carlo Menon
npj Digital Medicine.2024;[Epub] CrossRef - All That Glitters Is Not Gold: The Same Sleep Time, but Different Diabetogenic Outcomes
Bohye Kim, Obin Kwon
Endocrinology and Metabolism.2023; 38(1): 78. CrossRef - The Link Between Sleeping and Type 2 Diabetes: A Systematic Review
Ali Darraj
Cureus.2023;[Epub] CrossRef
- Attention to Innate Circadian Rhythm and the Impact of Its Disruption on Diabetes

- Diabetes, Obesity and Metabolism
- How Can We Adopt the Glucose Tolerance Test to Facilitate Predicting Pregnancy Outcome in Gestational Diabetes Mellitus?
- Kyeong Jin Kim, Nam Hoon Kim, Jimi Choi, Sin Gon Kim, Kyung Ju Lee
- Endocrinol Metab. 2021;36(5):988-996. Published online October 15, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1107
- 4,193 View
- 112 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We investigated how 100-g oral glucose tolerance test (OGTT) results can be used to predict adverse pregnancy outcomes in gestational diabetes mellitus (GDM) patients.
Methods
We analyzed 1,059 pregnant women who completed the 100-g OGTT between 24 and 28 weeks of gestation. We compared the risk of adverse pregnancy outcomes according to OGTT patterns by latent profile analysis (LPA), numbers to meet the OGTT criteria, and area under the curve (AUC) of the OGTT graph. Adverse pregnancy outcomes were defined as a composite of preterm birth, macrosomia, large for gestational age, low APGAR score at 1 minute, and pregnancy-induced hypertension.
Results
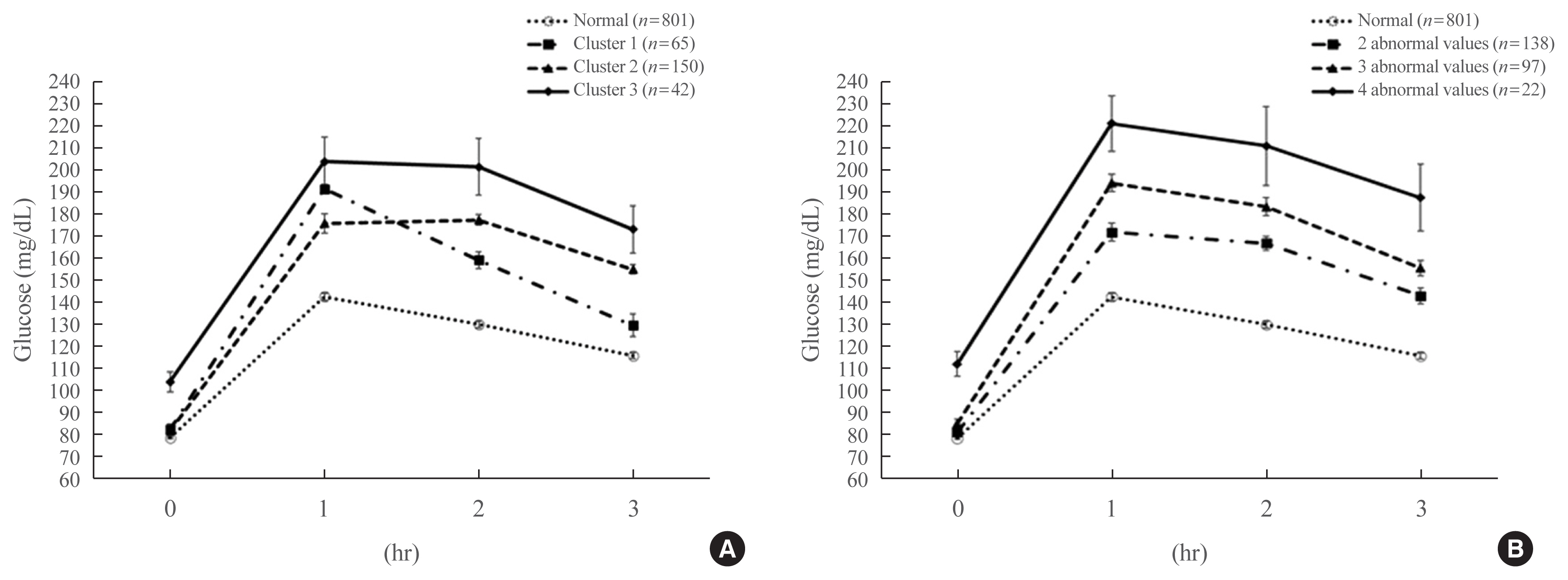
Overall, 257 participants were diagnosed with GDM, with a median age of 34 years. An LPA led to three different clusters of OGTT patterns; however, there were no significant associations between the clusters and adverse pregnancy outcomes after adjusting for confounders. Notwithstanding, the risk of adverse pregnancy outcome increased with an increase in number to meet the OGTT criteria (P for trend=0.011); odds ratios in a full adjustment model were 1.27 (95% confidence interval [CI], 0.72 to 2.23), 2.16 (95% CI, 1.21 to 3.85), and 2.32 (95% CI, 0.66 to 8.15) in those meeting the 2, 3, and 4 criteria, respectively. The AUCs of the OGTT curves also distinguished the patients at risk of adverse pregnancy outcomes; the larger the AUC, the higher the risk (P for trend=0.007).
Conclusion
The total number of abnormal values and calculated AUCs for the 100-g OGTT may facilitate tailored management of patients with GDM by predicting adverse pregnancy outcomes. -
Citations
Citations to this article as recorded by- Risk factors combine in a complex manner in assessment for macrosomia
Yi-Wen Wang, Yan Chen, Yong-Jun Zhang
BMC Public Health.2023;[Epub] CrossRef - Association of the Severity of Hypertensive Disorders in Pregnancy with Birthweight, Childhood Obesity, and Blood Pressure at Age 7
Yan Chen, Yiwen Wang, Yanjun Li, Guodong Ding, Yongjun Zhang
Nutrients.2023; 15(14): 3104. CrossRef
- Risk factors combine in a complex manner in assessment for macrosomia

- Miscellaneous
- The Status and Distinct Characteristics of Endocrine Diseases in North Korean Articles Published between 2006 and 2015
- Kyeong Jin Kim, Shin Ha, Yo Han Lee, Jung Hyun Noh, Sin Gon Kim
- Endocrinol Metab. 2018;33(2):268-272. Published online June 21, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.2.268
- 4,836 View
- 47 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Past decades of division have led to substantial differences in medical environments between South and North Korea. However, little is known about North Korea's medical status and research field, especially regarding endocrinology. In this study, we report the characteristics of North Korea's articles regarding endocrine-related diseases.
Methods Among the nine medical journals, articles published in
Internal Medicine between 2006 and 2015 were reviewed. A total of 2,092 articles were included; among them, 96 articles were associated with endocrinology. We analyzed these articles according to the disease categories they focused on and evaluated their features.Results Articles related to diabetes mellitus accounted for 55.2% (
n =53) and those to thyroid disease accounted for 28.1% (n =27). Other disease categories, including adrenal gland (n =1), pituitary gland (n =1), and osteoporosis (n =3), comprised minor portions. Regarding diabetes mellitus, more than half the articles (n =33) focused on treatment and complications. Experimental studies were conducted with old hypoglycemic drugs or natural substances for the treatment of hyperglycemia. Regarding thyroid disease, articles related to hyperthyroidism were the most common (51.9%,n =14), followed by thyroid nodule/cancer (18.5%,n =5). Unique article features were short length, no figures, and less than five references.Conclusion North Korea's endocrinology articles mainly focused on diabetes mellitus and thyroid disease. Persistent studies have been carried out in North Korea with dedication despite the poor medical environment. We hope that this study will be the beginning of mutual medical exchange and collaboration between North and South Korea.
-
Citations
Citations to this article as recorded by- Surgical Diseases in North Korea: An Overview of North Korean Medical Journals
Sejin Choi, Taehoon Kim, Soyoung Choi, Hee Young Shin
International Journal of Environmental Research and Public Health.2020; 17(24): 9346. CrossRef -
Endocrinology and Metabolism Has Been Indexed in MEDLINE: A Major Achievement
Won-Young Lee
Endocrinology and Metabolism.2019; 34(2): 138. CrossRef
- Surgical Diseases in North Korea: An Overview of North Korean Medical Journals

- Effects of Vildagliptin or Pioglitazone on Glycemic Variability and Oxidative Stress in Patients with Type 2 Diabetes Inadequately Controlled with Metformin Monotherapy: A 16-Week, Randomised, Open Label, Pilot Study
- Nam Hoon Kim, Dong-Lim Kim, Kyeong Jin Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Sin Gon Kim
- Endocrinol Metab. 2017;32(2):241-247. Published online June 23, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.2.241
- 4,632 View
- 94 Download
- 23 Web of Science
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Glycemic variability is associated with the development of diabetic complications through the activation of oxidative stress. This study aimed to evaluate the effects of a dipeptidyl peptidase 4 inhibitor, vildagliptin, or a thiazolidinedione, pioglitazone, on glycemic variability and oxidative stress in patients with type 2 diabetes.
Methods In this open label, randomised, active-controlled, pilot trial, individuals who were inadequately controlled with metformin monotherapy were assigned to either vildagliptin (50 mg twice daily,
n =17) or pioglitazone (15 mg once daily,n =14) treatment groups for 16 weeks. Glycemic variability was assessed by calculating the mean amplitude of glycemic excursions (MAGE), which was obtained from continuous glucose monitoring. Urinary 8-iso prostaglandin F2α, serum oxidised low density lipoprotein, and high-sensitivity C-reactive protein were used as markers of oxidative stress or inflammation.Results Both vildagliptin and pioglitazone significantly reduced glycated hemoglobin and mean plasma glucose levels during the 16-week treatment. Vildagliptin also significantly reduced the MAGE (from 93.8±38.0 to 70.8±19.2 mg/dL,
P =0.046), and mean standard deviation of 24 hours glucose (from 38±17.3 to 27.7±6.9,P =0.026); however, pioglitazone did not, although the magnitude of decline was similar in both groups. Markers of oxidative stress or inflammation including urinary 8-iso prostaglandin F2α did not change after treatment in both groups.Conclusion In this 16-week treatment trial, vildagliptin, but not pioglitazone, reduced glycemic variability in individuals with type 2 diabetes who was inadequately controlled with metformin monotherapy, although a reduction of oxidative stress markers was not observed.
-
Citations
Citations to this article as recorded by- What is Glycaemic Variability and which Pharmacological Treatment Options are Effective? A Narrative Review
Juan Miguel Huertas Cañas, Maria Alejandra Gomez Gutierrez, Andres Bedoya Ossa
European Endocrinology.2023; 19(2): 4. CrossRef - Glycemic Variability, Glycated Hemoglobin, and Cardiovascular Complications: Still a Dilemma in Clinical Practice
Antonio Ceriello, Ali A. Rizvi, Manfredi Rizzo
Advances in Therapy.2022; 39(1): 1. CrossRef - Contrasting Three Non-hypoglycemic Antidiabetic Drug Effects on Glycemic Control in Newly Diagnosed Type II Diabetes Mellitus: An Experimental Study
Abdulhamza Hmood, Mohammed Almasoody, Hameed Hussein Al-Jameel
Open Access Macedonian Journal of Medical Sciences.2022; 10(B): 506. CrossRef - Hypoglycemic agents and glycemic variability in individuals with type 2 diabetes: A systematic review and network meta-analysis
SuA Oh, Sujata Purja, Hocheol Shin, Minji Kim, Eunyoung Kim
Diabetes and Vascular Disease Research.2022; 19(3): 147916412211068. CrossRef - Influence of dipeptidyl peptidase-4 inhibitors on glycemic variability in patients with type 2 diabetes: A meta-analysis of randomized controlled trials
Shangyu Chai, Ruya Zhang, Ye Zhang, Richard David Carr, Yiman Zheng, Swapnil Rajpathak, Miao Yu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Comparison of Efficacy of Glimepiride, Alogliptin, and Alogliptin-Pioglitazone as the Initial Periods of Therapy in Patients with Poorly Controlled Type 2 Diabetes Mellitus: An Open-Label, Multicenter, Randomized, Controlled Study
Hae Jin Kim, In Kyung Jeong, Kyu Yeon Hur, Soo-Kyung Kim, Jung Hyun Noh, Sung Wan Chun, Eun Seok Kang, Eun-Jung Rhee, Sung Hee Choi
Diabetes & Metabolism Journal.2022; 46(5): 689. CrossRef - Effect of low dose allopurinol on glycemic control and glycemic variability in patients with type 2 diabetes mellitus: A cross-sectional study
Manal M. Alem
Heliyon.2022; 8(11): e11549. CrossRef - Effect of hydroxychloroquine on glycemic variability in type 2 diabetes patients uncontrolled on glimepiride and metformin therapy
Rajesh Rajput, Suyasha Saini, Siddhant Rajput, Parankush Upadhyay
Indian Journal of Endocrinology and Metabolism.2022; 26(6): 537. CrossRef - Effect of Dapagliflozin as an Add-on Therapy to Insulin on the Glycemic Variability in Subjects with Type 2 Diabetes Mellitus (DIVE): A Multicenter, Placebo-Controlled, Double-Blind, Randomized Study
Seung-Hwan Lee, Kyung-Wan Min, Byung-Wan Lee, In-Kyung Jeong, Soon-Jib Yoo, Hyuk-Sang Kwon, Yoon-Hee Choi, Kun-Ho Yoon
Diabetes & Metabolism Journal.2021; 45(3): 339. CrossRef - Comprehensive elaboration of glycemic variability in diabetic macrovascular and microvascular complications
Bao Sun, Zhiying Luo, Jiecan Zhou
Cardiovascular Diabetology.2021;[Epub] CrossRef - CGMS and Glycemic Variability, Relevance in Clinical Research to Evaluate Interventions in T2D, a Literature Review
Anne-Esther Breyton, Stéphanie Lambert-Porcheron, Martine Laville, Sophie Vinoy, Julie-Anne Nazare
Frontiers in Endocrinology.2021;[Epub] CrossRef - Efficacy and safety profile of sitagliptin, vildagliptin, and metformin in newly diagnosed type 2 diabetic subjects
Sahar Hossam Elhini, Amal K. Hussien, Ahmed Abd Elsamie Omran, Asmaa A. Elsayed, Haitham saeed
Clinical and Experimental Pharmacology and Physiology.2021; 48(12): 1589. CrossRef - Vildagliptin ameliorates renal injury in type 2 diabetic rats by suppressing oxidative stress
Fariba Aghahoseini, Alireza Alihemmati, Leila Hosseini, Reza Badalzadeh
Journal of Diabetes & Metabolic Disorders.2020; 19(2): 701. CrossRef - Small changes in glucose variability induced by low and high glycemic index diets are not associated with changes in β-cell function in adults with pre-diabetes
Kristina M. Utzschneider, Tonya N. Johnson, Kara L. Breymeyer, Lisa Bettcher, Daniel Raftery, Katherine M. Newton, Marian L. Neuhouser
Journal of Diabetes and its Complications.2020; 34(8): 107586. CrossRef - Comparison of the effects of gemigliptin and dapagliflozin on glycaemic variability in type 2 diabetes: A randomized, open‐label, active‐controlled, 12‐week study (STABLE II study)
Soo Heon Kwak, You‐Cheol Hwang, Jong Chul Won, Ji Cheol Bae, Hyun Jin Kim, Sunghwan Suh, Eun Young Lee, Subin Lee, Sang‐Yong Kim, Jae Hyeon Kim
Diabetes, Obesity and Metabolism.2020; 22(2): 173. CrossRef - Glycemic variability: adverse clinical outcomes and how to improve it?
Zheng Zhou, Bao Sun, Shiqiong Huang, Chunsheng Zhu, Meng Bian
Cardiovascular Diabetology.2020;[Epub] CrossRef - Anti-inflammatory properties of antidiabetic drugs: A “promised land” in the COVID-19 era?
Niki Katsiki, Ele Ferrannini
Journal of Diabetes and its Complications.2020; 34(12): 107723. CrossRef - Impact of long-term glucose variability on coronary atherosclerosis progression in patients with type 2 diabetes: a 2.3 year follow-up study
Suhua Li, Xixiang Tang, Yanting Luo, Bingyuan Wu, Zhuoshan Huang, Zexiong Li, Long Peng, Yesheng Ling, Jieming Zhu, Junlin Zhong, Jinlai Liu, Yanming Chen
Cardiovascular Diabetology.2020;[Epub] CrossRef - Visit-to-visit fasting plasma glucose variability is an important risk factor for long-term changes in left cardiac structure and function in patients with type 2 diabetes
Xixiang Tang, Junlin Zhong, Hui Zhang, Yanting Luo, Xing Liu, Long Peng, Yanling Zhang, Xiaoxian Qian, Boxiong Jiang, Jinlai Liu, Suhua Li, Yanming Chen
Cardiovascular Diabetology.2019;[Epub] CrossRef - Effect of dipeptidyl-peptidase-4 inhibitors on C-reactive protein in patients with type 2 diabetes: a systematic review and meta-analysis
Xin Liu, Peng Men, Bo Wang, Gaojun Cai, Zhigang Zhao
Lipids in Health and Disease.2019;[Epub] CrossRef - Efficacy and Safety of Pioglitazone Monotherapy in Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis of Randomised Controlled Trials
Fahmida Alam, Md. Asiful Islam, Mafauzy Mohamed, Imran Ahmad, Mohammad Amjad Kamal, Richard Donnelly, Iskandar Idris, Siew Hua Gan
Scientific Reports.2019;[Epub] CrossRef - Effect of DPP-IV Inhibitors on Glycemic Variability in Patients with T2DM: A Systematic Review and Meta-Analysis
Subin Lee, Heeyoung Lee, Yoonhye Kim, EunYoung Kim
Scientific Reports.2019;[Epub] CrossRef - Glycemic Variability: How to Measure and Its Clinical Implication for Type 2 Diabetes
Guillermo E. Umpierrez, Boris P. Kovatchev
The American Journal of the Medical Sciences.2018; 356(6): 518. CrossRef
- What is Glycaemic Variability and which Pharmacological Treatment Options are Effective? A Narrative Review


 KES
KES

 First
First Prev
Prev



